Cervical instability: what to do when a joint is unstable?
Cervical instability is a condition characterized by the reduced ability of the cervical vertebrae to maintain proper alignment, especially under stress during neck movements. This instability causes excessive vertebral motion, which can lead to pain, discomfort, and, in more severe cases, impair the functionality of the nerves or spinal cord.
Cervical spine instability, particularly atlanto-occipital and atlanto-axial instability, can be caused by various factors, including physical trauma, age-related degenerative processes, rheumatic diseases, cervical spine surgeries, or congenital abnormalities in the vertebral structures. Symptoms can vary in severity and include neck pain, stiffness, limited range of motion, headaches, dizziness, crepitus (crackling noises) during neck movement, and, in some cases, neurological symptoms such as tingling, weakness, or sensory changes in the limbs.
The diagnosis of cervical instability requires a thorough clinical evaluation supported by imaging techniques such as X-ray, MRI, and CT scan. These tests allow for the analysis of vertebral alignment, ligament integrity, and the condition of intervertebral discs, highlighting any abnormalities or injuries.
To achieve an accurate diagnosis of cervical instability, it is necessary to acquire dynamic images by performing scans with the head in different positions. This approach can detect instability not visible in static images, which might be misleading and fail to reveal the true condition. Additionally, it is important to note that many radiologists may lack the experience or specific training required to properly identify cervical spine instability, emphasizing the need for specialized attention in this area.
Instability after a whiplash injury
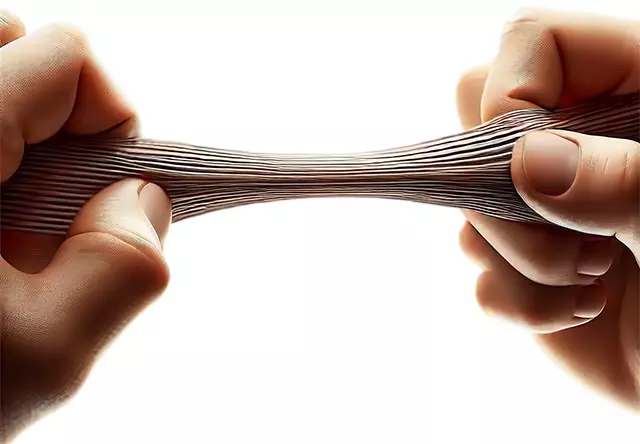
Following an accident with whiplash that caused stretching of the joint capsule and/or ligaments, the joint may exhibit excessive laxity, meaning the involved vertebrae can move more than normal in relation to one another or the Atlas relative to the occiput, making the joint unstable during movement. This situation leads to abnormal variable compressions of adjacent structures such as blood vessels and nerves. Inappropriate cervical postures maintained over time can also cause adaptation and elongation of the ligaments and joint capsules, as seen in cases of cervical straightening.
In the following video, it is possible to observe at the 2:10 mark how, during lateral flexion of the head, the C2 spinous process rotates abnormally, while the Atlas tends to slide laterally, highlighting significant joint instability.
Joint instability is difficult to identify through static images. A single "snapshot" is not sufficient, as the instability primarily manifests during cervical spine movement. For an accurate diagnosis, a dynamic approach is necessary, similar to a "video" of the moving structures. Alternatively, static images can be captured in different joint positions to reveal potential alterations. The examination shown in the video uses an X-ray technology called fluoroscopy or Digital Motion X-ray (DMX), which allows for visualization of cervical structures in motion, providing a more detailed and accurate analysis than traditional static images.
The risk of joint tissue hyperlaxity
It is widely recognized that muscle strengthening contributes to increased joint stability. However, when the tissues responsible for maintaining joint integrity, such as ligaments and capsules, do not provide adequate support, physical exercise may exert inappropriate stress on the involved joints, further aggravating the condition. Therefore, in case of doubt, it is essential to check for the presence of joint instability caused by torn or excessively lax ligaments before starting an exercise program.
Prolotherapy to address joint instability
The term "prolotherapy" comes from "proliferation therapy," coined in the 1950s by Dr. George Hackett, an American orthopedic surgeon.
Prolotherapy involves the injection of an irritant solution, such as dextrose, directly into the injured area to stimulate the body's natural healing process for tissues.
Dextrose triggers a local inflammatory response that induces a self-repair reaction with the formation of new connective tissue at the injection site. This process helps strengthen damaged tissues, restore joint stability, and increase the tensile strength of stabilizing structures, such as ligaments, tendons, and joint capsules.
Prolotherapy is considered an effective, generally safe method with minimal side effects, which in many cases can avoid the need for surgery. If you suffer from generalized ligament laxity unrelated to an accident, prolotherapy might be less effective because your body produces little collagen, and inducing tissue inflammation may limit the production of new elastic tissue.
Collagen is an essential component for the strength and elasticity of connective tissues, and its adequate production is crucial for ligament repair and reinforcement. To stimulate collagen synthesis, it is important to ensure sufficient intake of key nutrients, including vitamin C and vitamin D. High doses of vitamin C (10-15 g per day), in addition to being a powerful antioxidant, play a fundamental role in collagen production, promoting the formation and maintenance of healthy connective tissues. For this reason, those undergoing prolotherapy or seeking to improve the health of their connective tissues may benefit from learning about the advantages of vitamin C and how to increase its intake through diet or supplements.
Although prolotherapy is less well-known compared to other medical interventions such as surgery or medication use, it has gained attention for its effectiveness in treating certain musculoskeletal conditions, particularly those involving ligament laxity. Its simplicity and relatively low cost may make it less prominent in the landscape of therapeutic options traditionally promoted, which often involve greater economic benefits for the healthcare sector.
The use of ultrasound in prolotherapy offers a significant advantage by enabling precise localization of the treatment area. This non-invasive imaging method helps identify the exact point for solution injection, improving treatment efficacy while reducing the risks associated with imprecise injections. When performing prolotherapy on specific vertebrae like the Atlas and axis, precision is crucial due to the complexity and sensitivity of the cervical region.
Below is a video showing how prolotherapy is performed on C1:
PICL: Percutaneous Implantation of Cervical Ligaments
The PICL procedure (Percutaneous Implantation of Cervical Ligaments) is an advanced, minimally invasive surgical technique developed to repair damaged ligaments in the cervical region, particularly those stabilizing the joint between the occipital bone (C0), the Atlas (C1), and the axis (C2). This procedure is distinguished by its transoral approach, which allows direct access to and treatment of the injured ligaments without the need for external fixators, which can significantly limit head mobility.
The PICL technique offers several advantages over traditional cervical stabilization methods, which often involve bulky external devices and long recovery periods. With PICL, recovery time is typically shorter and less painful, and the procedure aims to preserve or even improve cervical region mobility.
Due to its minimally invasive nature, PICL reduces the risk of infections and other post-operative complications associated with more invasive interventions. However, it is essential that this procedure be performed by surgeons experienced in minimally invasive techniques and in managing cervical spine pathologies, as the cervical region is complex and requires extreme surgical precision to avoid damage to nerves or other vital structures.
What People Say About Us
Beware of those who disguise a simple cervical manipulation as Atlas realignment and those who offer low-quality imitations of our method. The results speak for themselves: over 10,000 testimonials and reviews in various languages make us unique. Click to discover opinions, ratings, and authentic experiences shared by those who have experienced Atlas correction with Vibro-Resonance AtlantoMed:



