Vagus nerve dysfunction
The dysfunctions that can arise from VAGUS NERVE compression are numerous and can affect the entire body, either directly or indirectly, as this nerve is connected to most organs.
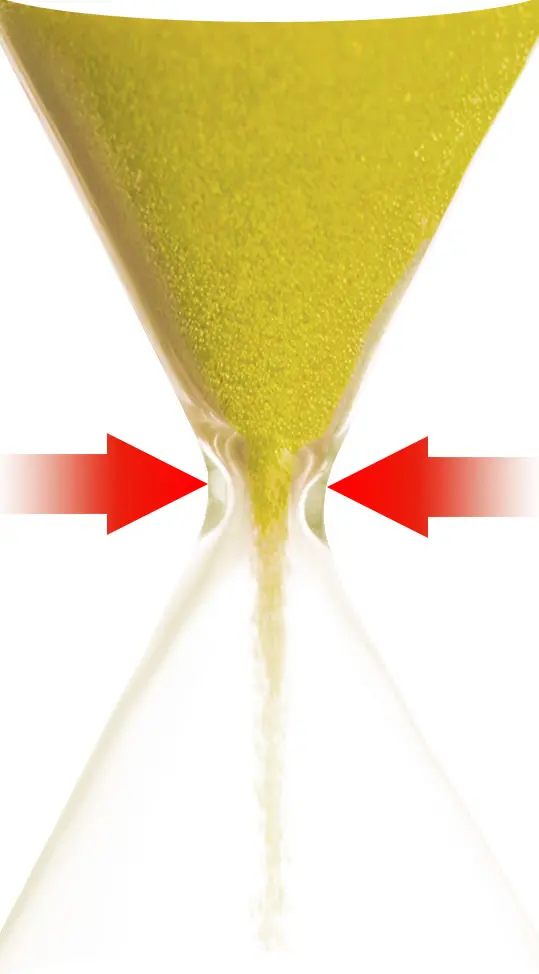
As highlighted on the page dedicated to the autonomic nervous system, among the various insidious effects of Atlas misalignment is the compression of various nerve bundles, including the vagus nerve. This "strangulation" interferes with the normal flow of electrical impulses along the nerves, altering their intensity or, in more severe cases, completely blocking transmission. This compromises the functions these nerves perform, especially when the compression is significant and persistent.
Imagine the consequences on the organs connected to these nerves, whose function and regulation depend on the signals they receive. It's similar to disconnecting the antenna cable that transmits the signal to your TV: the result is the same. Although the body is equipped with sophisticated adaptation and compensation mechanisms to mitigate malfunctions, what happens if chronic vagus nerve compression exceeds these capacities?
Vagal compression: a stealthy condition
Let me explain with an analogy. The silent compression of nerves that regulate organs is to the organs what a spinal nerve injury is to the body: a paralysis.
Unlike a spinal cord injury, which causes total or partial paralysis that is immediately recognizable, the "paralysis" of organs caused by vagus nerve compression is much more insidious. The effects can be so subtle and widespread that even an experienced doctor may not easily associate them with vagus nerve dysfunction. When the vagus nerve is compromised, the connected organs do not stop functioning suddenly but begin to show malfunctions that often go unnoticed or are attributed to other causes.
The importance of the vagus nerve
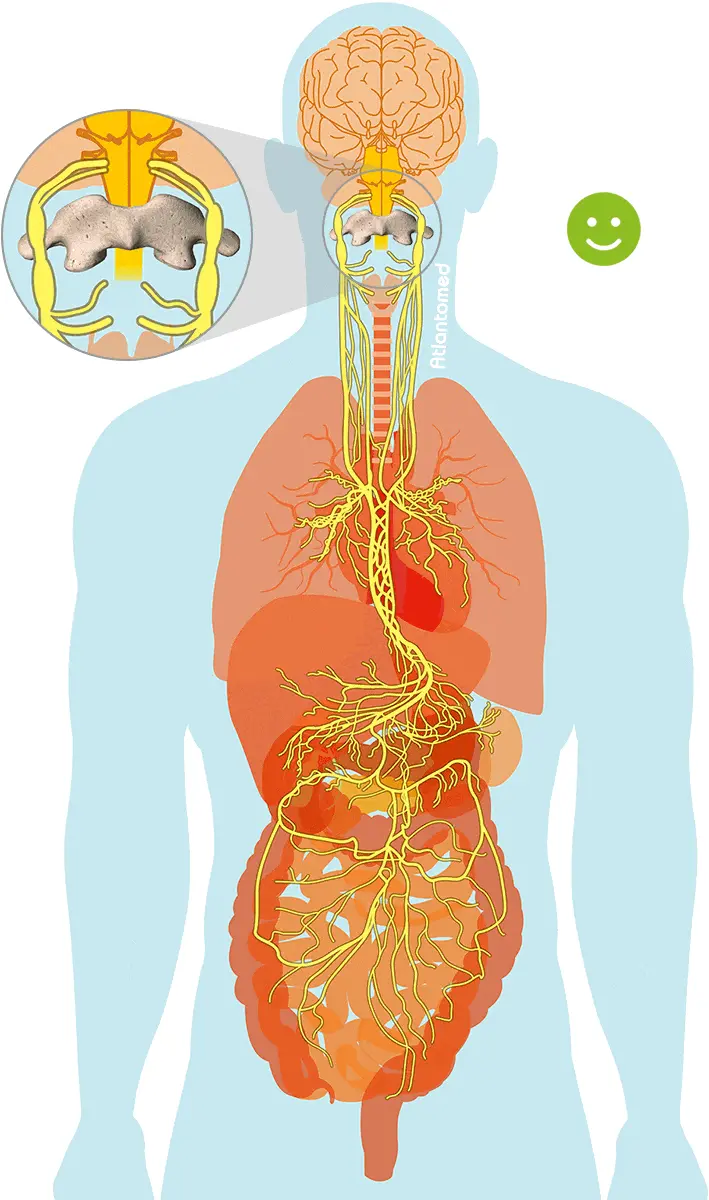
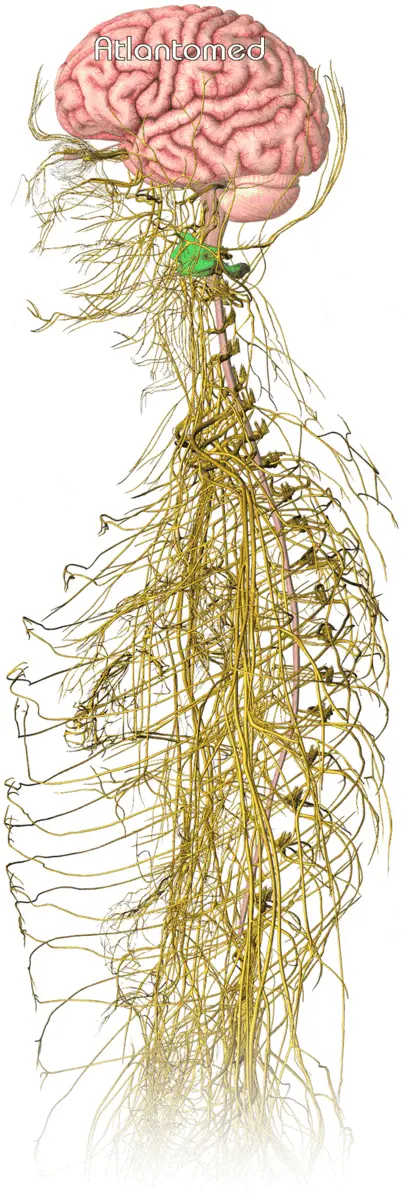
The vagus nerve, the tenth cranial nerve, belongs to the autonomic nervous system and is the longest, most branched, and most important cranial nerve of the parasympathetic nervous system.
The vagus nerve is involved in regulating the functions of almost all internal organs. It innervates the larynx, pharynx, upper part of the esophagus, part of the external auditory system, heart, lungs, stomach, and intestines.
With a diameter of 2-3 mm at the neck level, the vagus nerve runs alongside the carotid artery and the internal jugular vein, positioned right in front of the Atlas vertebra.
Functions of the vagus nerve
VAGUS NERVE (Nervus vagus)
- regulates appetite
- regulates sweating
- participates in mood regulation
- stimulates gastric acid production
- contributes to heart rate regulation
- controls intestinal movements during digestion (peristalsis)
Another important function of the vagus nerve is to stimulate the release of bile from the gallbladder. Bile is essential in digestive processes, facilitating the absorption of fats and enabling the elimination of unwanted substances such as excess cholesterol and toxins.
The pancreas is also negatively affected by an irritated vagus nerve.
Symptoms of vagus nerve compression
Depending on the severity and type of Atlas displacement from its optimal position, pressure and irritation of the vagus nerve and/or other cranial nerves may occur.
When vagus nerve functionality is compromised (even by cervical osteoarthritis), various symptoms may arise:
BEFORE
AFTER ATLANTOMED
- thyroid problems
- headache – insomnia
- nausea – stomach acidity
- dizziness – Meniere's disease
- cervical pain – neck stiffness
- chronic constipation – unexplained diarrhea
- habitually cold hands or feet
- irregular or accelerated heartbeat
- tachycardia (accelerated heartbeat)
- difficulty swallowing – lump in the throat
- facial redness – excessive sweating
- sudden fainting (vasovagal syncope)
- numbness or tingling of the scalp
Vagus nerve and epileptic seizures
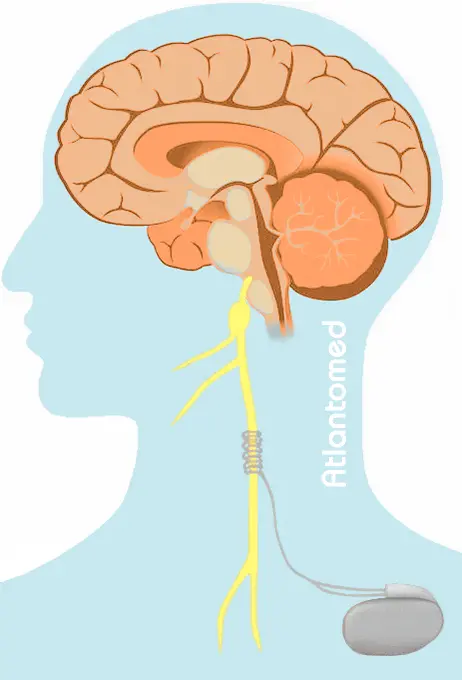
Among the dysfunctions associated with the vagus nerve, we can also mention epilepsy. The realignment of the Atlas can have a positive impact on epilepsy, as demonstrated by several cases treated with AtlantoMed.
The conventional medical approach to severe epileptic seizures involves surgical intervention on the LEFT vagus nerve, either by cutting it (vagotomy) or inhibiting its function through electrical impulses generated by an implanted stimulator. From our point of view, this is an invasive procedure bordering on barbarity.
The LEFT vagus nerve is statistically the most affected by Atlas misalignment. Is this merely a coincidence? This aspect certainly deserves more attention and further research.
Vagus nerve and fainting (vasovagal syncope)
One of the most striking dysfunctions that often resolves spontaneously after Atlas correction with the AtlantoMed method is sudden fainting, also known as vasovagal syncope.
Lipothymia, also called pre-syncope, is a condition characterized by a sensation of imminent loss of consciousness and extreme weakness, which may precede vasovagal syncope or resolve without leading to fainting. These manifestations are related to an abnormal response of the autonomic nervous system, causing a sudden reduction in blood flow to the brain, which may already be compromised if the first two cervical vertebrae are misaligned.
Main triggering factors:
- Posture: standing for long periods or quickly moving from a lying to an upright position (orthostatic hypotension), especially if the basic posture is compromised.
- Physical stimuli: tilting the neck backward, such as when looking up, or pressure on the neck area can stimulate the vagus nerve.
- Gastrointestinal stimuli: such as coughing, swallowing, urination, or defecation (situational syncope).
- Intense emotional stimuli: fear, pain, stress, or anxiety can trigger a vasovagal response.
- Pain or physical trauma: painful experiences, such as an injection or injury, can trigger syncope.
- Excessive fatigue: physical or mental exhaustion can contribute.
- Environmental factors: hot, crowded, or poorly ventilated environments can lead to a drop in blood pressure.
- Dehydration: a reduction in circulating blood volume can facilitate fainting.
The listed triggering situations represent only the immediate events of an already precarious underlying condition. Among these, Atlas misalignment is probably the most significant cause, as after the correction of the first vertebra, syncope has often not reoccurred, despite previous medical diagnoses and treatments having failed.
In addition to the Atlas, there may also be other mechanical issues in the cervical spine capable of causing the same compression effect on the vagus nerve. For example: congenitally deformed or displaced vertebrae due to ligament laxity or joint capsule damage from accidents or whiplash, or cervical osteoarthritis that has degenerated the tissues.
Compression of the vagus nerve by the Atlas has an effect comparable to a faulty contact in an electrical circuit: during the movement of wires, the unstable contact between conductors generates sparks. Similarly, suddenly compressing the vagus nerve, which is already in a precarious functional state, especially during neck extensions, causes a "short circuit."
When the neck returns to a neutral position and the pressure on the nerve decreases, the nerve suddenly resumes transmitting signals, causing hyperactivation. This process leads to a rapid decrease in heart rate (bradycardia) and a sudden drop in blood pressure (hypotension), resulting in loss of consciousness.
Observing cases of sudden fainting caused by head movements, it is clear that fainting always occurs an instant after the neck movement.
To delve deeper into this dynamic, we asked the girl in the video, who suffered from frequent fainting episodes, to constantly record herself with her phone on a tripod while at home. The video analysis clearly shows that fainting always occurs right after performing certain movements, but never during them:
In the process leading to syncope, it is hypothesized that blood vessels, including the vertebral artery and accompanying veins along its course, as well as the jugular vein, which is already in a precarious condition, are further compressed by specific movements.
A straightening of the cervical spine could aggravate the situation, further lowering the threshold for syncope.
The success of AtlantoMed in cases of syncope is likely due to the simultaneous improvement of several critical and unfavorable conditions.
Testimonials about sudden fainting and the Atlas vertebra:
Vagus nerve and conventional medicine
When the vagus nerve is mentioned in medical literature, it is usually done briefly and, I would add, vaguely: "...the vagus nerve passes here, is structured like this, ...the vagus nerve performs this or that function". However, the connection between the vagus nerve and the associated problems is rarely given adequate consideration.
In fact, even when dysfunctions are clearly attributable to a vagus nerve dysfunction, it is rarely recognized as the culprit, even in cases where its involvement is evident. One example is that, although medical literature mentions the vagus nerve as a possible cause of stomach acidity (it is even cited in Wikipedia under the section on dysfunctions related to the vagus nerve), doctors always prescribe medications to neutralize the acid, without ever investigating the vagal problem.
Such examples are numerous. It is well known that conventional medicine prefers to focus on symptoms rather than investigate the root cause. Cause and effect are often reversed, as it is more economically profitable to treat symptoms rather than explore possible correlations with the vagus nerve.
The reason for this apparent "oversight" probably lies in the fact that there is no pill to "cure" the vagus nerve.
With the AtlantoMed method, vagus nerve compression can be effectively resolved. Those who have undergone the treatment often report significant improvements in vagal dysfunctions. Only after resolving the issue does one realize the extensive range of ailments linked to vagus nerve compression. This leads to the conclusion that the repercussions of a compromised vagus nerve are much deeper and more far-reaching than previously thought.
Video interviews about vagus nerve dysfunctions
You can get an idea of what has been mentioned by listening to the testimonials of people treated with the AtlantoMed method in relation to the vagus nerve.
Accounts after Atlas realignment
Some testimonials from the forum
- Silvia17: Labyrinthitis and vagus nerve dysfunctions
- Melfi Raffaele: Solution to my VAGAL SYNDROME
- Fran: Cervical issues, headaches, and other VAGUS NERVE dysfunctions
- Marco1990italia: Vagal dysfunctions: dizziness and gastrointestinal problems
- Other testimonials: Vagus nerve (vasovagal) and other dysfunctions
What People Say About Us
Beware of those who disguise a simple cervical manipulation as Atlas realignment and those who offer low-quality imitations of our method. The results speak for themselves: over 10,000 testimonials and reviews in various languages make us unique. Click to discover opinions, ratings, and authentic experiences shared by those who have experienced Atlas correction with Vibro-Resonance AtlantoMed:



